Decades of research highlight certain community-level tools and practices that work to reduce death and disease, particularly among women and children. See chart for seven evidence-based solutions for top causes of preventable deaths among women and children that can be delivered at the community level >>
However, these proven solutions in isolation cannot reach those who need them most. Physical tools such as bednets need to be delivered, behaviors such as breastfeeding need to be adopted, and practices such as home visitation need to be carried out by qualified health workers. That is why community health organizations around the world, from rural villages in Malawi to crowded urban slums in Bangladesh, are engaged in on-the-ground efforts to reach vulnerable communities with these proven solutions.
One way these organizations achieve this is by recruiting local people to become “community health workers” (CHWs) who often serve as the backbone to an effective community health program. Although the variety of services CHWs provide varies considerably by region and type of program, they all in some way help teach their communities about life-saving healthy habits such as prenatal care, nutrition, vaccines, and proper sanitation and hygiene. In return, effective programs provide CHWs with training, adequate supervision, incentives (monetary or otherwise), and integration into the larger health system.
Community-based health programs and their CHWs deliver health services at the neighborhood and household level, using the following five principles:
- Local adaptation: Local health data is systematically collected and used to address the community’s most pressing health needs.
- Community participation: Community members participate in designing and delivering programs.
- Accessibility: Services are brought close to or into the homes of community members through outreach by CHWs, mobile clinics, and health educators.
- Comprehensiveness: Care is provided as a comprehensive package of preventative and treatment interventions through trusted, well-trained health workers.
- Integration: Services are linked to a broader health system (such as through referral networks) and strong partnerships with other stakeholders such as local governments.
In practice, this means that nonprofits provide health interventions such as physical tools (bednets, vaccines, medications) and promote healthy behaviors (such as breastfeeding and handwashing), through delivery methods such as home visitation by CHWs, group meetings of community residents, and mobile clinics. These approaches are especially important for isolated or vulnerable communities with limited access to clinical facilities due to distance, money, and/or social factors such as cultural discrimination, mistrust, and language barriers.
Health issue
Diarrheal Diseases
Malaria
Pneumonia
Newborn Health
Maternal Health
Malnutrition
Vaccine-preventable diseases
Solution (includes both prevention & treatment)
- Water, sanitation & hygiene (WASH) interventions, such as providing clean water, proper sanitation, and hygiene education
- Oral Rehydration Solution (ORS) and zinc, a simple solution of salt and sugar made with clean water
- Long-lasting insecticide-treated mosquito nets (ITNs) + indoor residual spraying (IRS)
- Oral antimalarial drugs (artemisinin-based combination therapy, or ACT) and rapid diagnostic tests (RDTs)
- Pneumococcal vaccine, which protects individuals from developing a deadly type of pneumonia
- Community case management (CCM) of pneumonia, a strategy to diagnose and treat childhood pneumonia outside the hospital
- Newborn care package, a suite of practices including kangaroo mother care (skin-to-skin) and clean delivery
- Breastfeeding promotion
- Newborn resuscitation by skilled providers at birth
- Home visitation after birth with prompt treatment of infections
- Prenatal care to decrease risk
- Rapid referral for complications such as hemorrhage & sepsis during childbirth
- Skilled birth attendants who are trained to manage normal pregnancies and childbirth
- Breastfeeding promotion
- Access to healthy foods (adequate nutrition)
- Ready-to-use therapeutic food (RTUF) for those with malnutrition
-
Childhood vaccines for measles, diphtheria, pertussis, tetanus, polio, and rotavirus
While some health interventions are not appropriate to provide at the community level (e.g., emergency C-sections), those that are have the potential to save millions of additional children’s lives when delivered using community-based approaches to health. These community-based strategies also work effectively in tandem with clinic and hospital settings. For example, a CHW can screen children in the community for malnutrition, and refer severely malnourished children to a local hospital for necessary care.
To date, such community-based approaches have been applied to and studied most in regards to preventing maternal and child deaths, because women and children are often the most vulnerable members of society. However, more nonprofits are extending the application of these approaches further, such as by managing chronic diseases, as community health needs evolve.
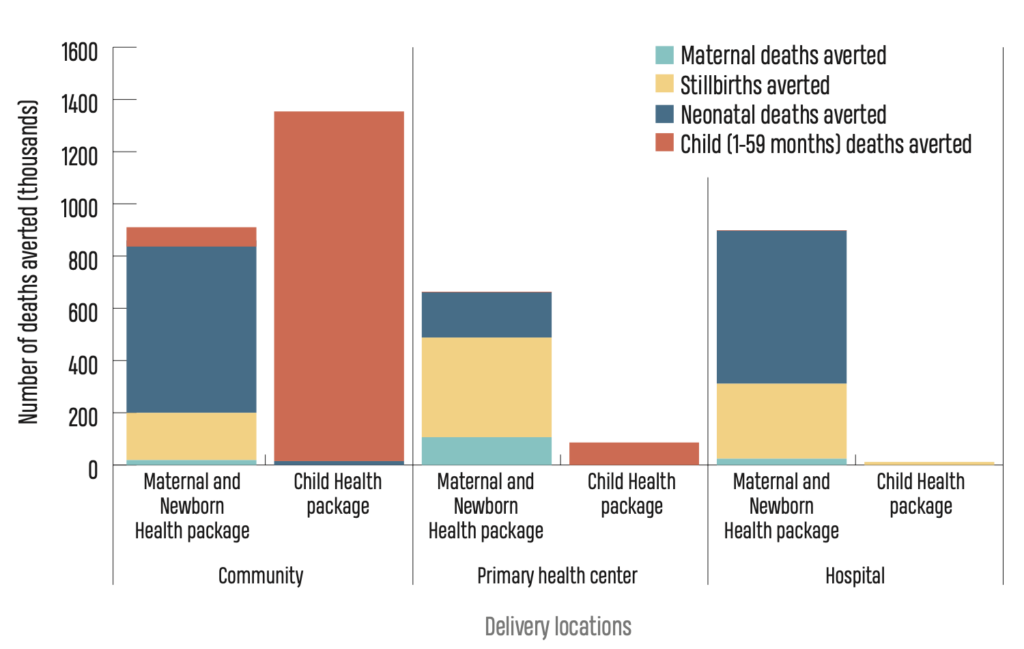
Delivering health interventions in community settings is particularly important because clinical settings such as hospitals and primary health centers are limited in their reach and capacity and require more specialized medical expertise. Community-based health delivery complements clinical approaches by reaching people where they are, such as in their homes.
The potential impact of scaling up a community-based approach has been demonstrated: Based on decades of research, leading public health academics and the World Health Organization estimate that as many as 4 million additional lives of mothers and children could be saved each year if low-income countries increased access to a package of essential health interventions to 90% of their target populations.
This package includes interventions for maternal and child health, such as promoting breastfeeding, labor with a skilled birth attendant, screening for severe acute malnutrition, oral antibiotics for newborns with pneumonia, and administering immunizations. See chart which shows that of the additional child deaths that could be averted with such increased access, 90% can be prevented at the community level.
Lives That Could Be Saved
Hospitals and primary health centers have no doubt improved maternal and child health. Yet, more lives can be saved by scaling up high impact community interventions than other clinic and hospital interventions combined. The community level is where the top causes of child death (such as pneumonia, malaria, and diarrhea) can most effectively be prevented and treated. A child health package consisting of interventions delivered through community-based approaches can avert thousands of deaths.
